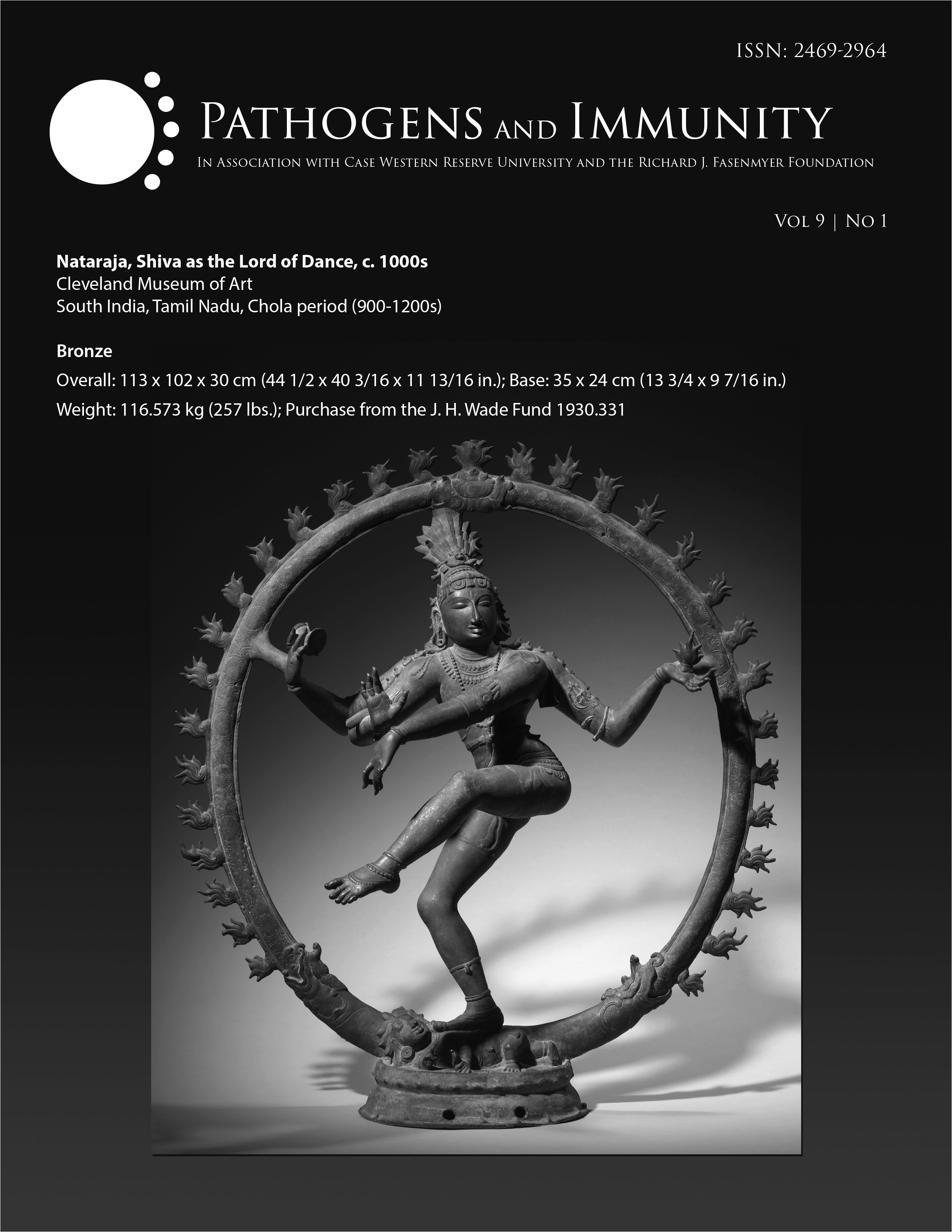
About Pathogens and Immunity
Pathogens and Immunity is a free, open-access journal committed to advancing human immunology and infectious disease research through rigorous, transparent, and accessible scientific research.
- We consider original research articles that offer meaningful new insights into human health and disease.
- Reviews and commentaries are published by invitation only; unsolicited reviews or commentaries are not considered.
- Any use of artificial intelligence (AI) in the development of a manuscript must be fully disclosed. Authors must state which tools were used, how and where they were applied, and provide appropriate citations within the manuscript.
Read more | See submission guidelines
Expert Exchange Interviews
Read the transcript. Watch the video. |
Read the transcript. Watch the video. |
Read the transcript. Watch the video. |
Read the article. |
Read the transcript. Watch the video. |

Read the transcript. Watch the video. |

Read the transcript. Watch the video |

Read the transcript. Watch the video, part 1. and part 2 |

Read the transcript. Watch the video. |

Watch the video. |
Read the transcript. Watch the video. |
Read the transcript. Watch the video |
See all Expert Exchange Interviews
Current Articles
Volume 11, Issue 1
2025 Conference on Bacteriophages: Biology, Dynamics, and Therapeutics
Published: February 9, 2026 | 10.20411/pai.v11i1.942
Eating Away at Antibiotic Resistance – Is Phage Therapy Our Future?
Published: February 9, 2026 | 10.20411/pai.v11i1.967
Gastrointestinal Mucosal Disruptions During ART-Treated SIV/Plasmodium fragile Co-Infection
Published: February 3, 2026 | 10.20411/pai.v11i1.854
Characterization of Distinct Monocyte Subtypes and Immune Features Associated with HIV, Tuberculosis, and Coronary Artery Disease in a Ugandan Cohort Using Mass Cytometry
Published: January 29, 2026 | 10.20411/pai.v11i1.945
Long-Term Follow-Up After Fecal Microbiota Transplantation via Freeze-Dried Capsules for Recurrent Clostridioides difficile Infection
Published: January 21, 2026 | 10.20411/pai.v11i1.868
Interested in submitting to this journal?
- Online submissions are rapid (less than 5 minutes).
- There are no charges to authors for submission or publication.
- We review submissions in any National Library of Medicine-approved format.
- Manuscripts only need to be revised to fit the journal format if accepted.
- Reviewers receive a modest cash payment for reviews completed in a timely manner.
- Authors may, if they wish, provide unedited complete reviews from another named journal together with their response to these critiques that may assist in the review.
- Articles are indexed on PubMed, PubMed Central, Scopus, Google Scholar, and the Directory of Open Access Journals.
We recommend that you review the About the Journal page for the journal's policies, as well as the Author Guidelines.