Sarah N. Redmond1, Sandra Y. Silva2, Brigid M. Wilson3, Jennifer L. Cadnum4, Curtis J. Donskey1,3
1
Case Western Reserve University School of Medicine; Cleveland, Ohio
2
Clinical and Translational Science Program; School of Medicine; Case
Western Reserve University; Cleveland, Ohio
3
Geriatric Research, Education, and Clinical Center; Louis Stokes Cleveland
VA Medical Center; Cleveland, Ohio
4
Research Service; Louis Stokes Cleveland VA Medical Center; Cleveland, Ohio
Curtis J. Donskey
Geriatric Research, Education, and Clinical Center
1110W, Louis Stokes Cleveland VA Medical Center
10701 East Boulevard, Cleveland, Ohio 44106
Phone: 216-791-3800 ext. 4788
Fax: 216-229-8509
Curtis.Donskey@va.gov
Background: Fluoroquinolone restriction has been proposed as a control measure for Clostridioides difficile infection (CDI) outbreaks associated with fluoroquinolone-resistant ribotype 027 strains. However, relatively few reports of fluoroquinolone restriction interventions have evaluated the impact on C. difficile strain types and fluoroquinolone resistance.
Methods: In a hospital and affiliated long-term care facility (LTCF), antimicrobial stewardship and environmental cleaning interventions were implemented between 2009 and 2018, and C. difficile isolates during this period (~20 per year) were ribotyped and tested for fluoroquinolone resistance by moxifloxacin minimum inhibitory concentrations (MICs). Pearson’s correlation coefficient was used to assess the association between use of fluoroquinolones and the percentage of CDI cases due to the 027 strain over time.
Results: Between 2009 and 2018, prescribing of fluoroquinolones to inpatients decreased by 43%, coinciding with significant reductions in the healthcare-associated CDI rates in the hospital and LTCF and a decline in the percentage of C. difficile isolates that were ribotype 027 from 70% to 10%. Ninety-five percent of ribotype 027 and 6% of non-027 isolates were moxifloxacin resistant. Hospital fluoroquinolone use was strongly correlated with the incidence of hospital-associated CDI (r = 0.79, 95% confidence interval, 0.31-0.95), but LTCF fluoroquinolone use was not correlated with LTCF-associated CDI (r = 0.29, 95% confidence interval, -0.43-0.77). During the study period, there were statistically significant downward trends in the use of penicillins, intravenous vancomycin, carbapenems, and clindamycin.
Conclusion: Our results provide support for fluoroquinolone restriction as a control measure for CDI outbreaks due to fluoroquinolone-resistant 027 strains, but also highlight the need for randomized trials as factors such as reduction in other antibiotic classes and improved cleaning may also impact CDI rates.
Keywords: fluoroquinolone; Clostridioides difficile; antimicrobial stewardship; environment; long-term care facility
During the past 2 decades, the fluoroquinolone-resistant ribotype 027 strain of Clostridioides difficile has been associated with large outbreaks in North America and Northern Europe [1]. Evidence from mouse models and in patients suggests that exposure to fluoroquinolones results in selective pressure favoring colonization and infection with 027 strains [2-3]. Thus, restriction of fluoroquinolones has been proposed as a control measure for outbreaks associated with 027 strains [2-4]. In England, a national program that included reductions in the use of fluoroquinolones and cephalosporins in conjunction with improved infection control practices resulted in reductions in CDI that were driven by substantial decreases in fluoroquinolone-resistant genotypes, including 027 [4]. However, fluoroquinolone restriction has not always been similarly effective. For example, in a tertiary care hospital a significant reduction in fluoroquinolone prescribing did not reduce CDI or the proportion of cases due to 027 strains [5].
Given the importance of CDI as a public health problem, there is a need for additional evidence regarding the impact of fluoroquinolone prescribing on CDI rates and infections due to the 027 strain. At the Cleveland VA Medical Center, antimicrobial stewardship interventions during the past decade have included efforts to reduce overuse of fluoroquinolones, particularly in the affiliated long-term care facility (LTCF). Here, we tested the hypothesis that reductions in fluoroquinolone use in the hospital and LTCF would be associated with a reduction in the proportion of cases due to ribotype 027 strains.
The institutional review board at the Cleveland VA Medical Center approved all study activities. Informed consent was waived.
The Cleveland VA Medical Center includes a 215-bed hospital and a 250-bed LTCF. Since January 2009, stool specimens testing positive for toxigenic C. difficile have been saved and stored at -80 °C. Beginning in January 2009, an antimicrobial stewardship intervention in the LTCF reduced total antibiotic use with reductions in several classes of antibiotics, including fluoroquinolones [6]. In the hospital, antimicrobial stewardship interventions have included education focused on reducing the use of antibiotics considered high-risk for CDI, including fluoroquinolones, and reducing treatment of asymptomatic bacteriuria. Beginning in 2011, the infection control program implemented a cleaning and disinfection intervention that was effective in reducing environmental contamination with C. difficile [7].
To assess the impact of the stewardship interventions on fluoroquinolone use, we used pharmacy databases to assess systemic fluoroquinolone use measured as days-of-therapy per 1,000 patient-days in the hospital and LTCF. In the hospital, we also examined the use of cephalosporins (ceftriaxone, cefazolin, cefepime, cefoxitin), penicillins (ampicillin, ampicillin/sulbactam, piperacillin/tazobactam,), vancomycin (intravenous only), carbapenems (meropenem, imipenem-cilastatin, ertapenem), clindamycin, and macrolides (azithromycin, clarithromycin). CDI rates were measured as healthcare facility-associated (HCFA) CDI cases per 10,000 patient-days for the hospital and LTCF.
To estimate the percentage of HCFA CDI cases due to the 027 strain, we cultured the first 5 individual patient stool specimens from each quarter of the year (a total of 20 per year) from 2009 through 2018 for toxigenic C. difficile [5, 7]. PCR ribotyping using capillary gel electrophoresis and fluorescent ribotyping was performed as previously described [5]. All isolates were tested for moxifloxacin susceptibility by broth dilution minimum inhibitory concentrations (MIC). Strains were classified as susceptible (MIC < 2ug/uL), intermediate (MIC 4ug/uL), resistant (MIC > 8ug/uL), and highly resistant (MIC > 32ug/uL) [2].
We calculated the percentage of CDI isolates each year that were due to the 027 strain. We used Pearson’s correlation coefficient to assess the association between fluoroquinolone use and the percentage of CDI cases due to the 027 strain over time. The non-parametric Mann-Kendall test was used to detect monotone trends in the CDI rate and use of antibiotics. All analyses were performed using R version 3.5.1 statistical software (The R Foundation for Statistical Computing, Vienna, Austria).
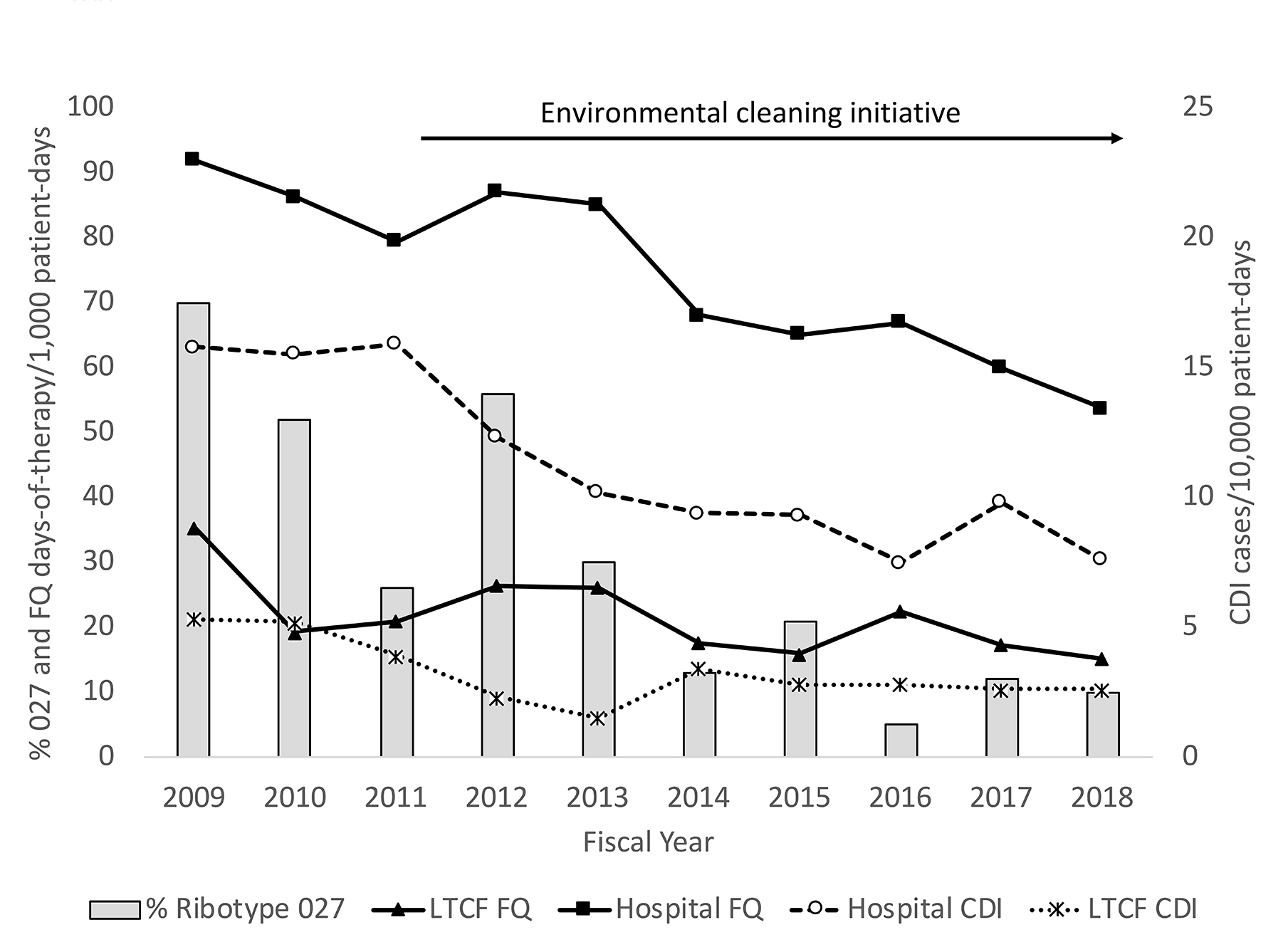
Figure 1 shows the rates of hospital- and LTCF-associated CDI cases and fluoroquinolone use as well as the percentage of C. difficile isolates that were ribotype 027. The HCFA CDI rate decreased in the hospital and LTCF by 52% and 51%, respectively. Prescribing of fluoroquinolones to inpatients decreased by 43% overall from 2009 to 2018, with 57% and 42% reductions in the hospital and LTCF, respectively. The reduction in fluoroquinolone use coincided with a decline in percentage of C. difficile isolates that were ribotype 027 from 70% to 10%. The decrease in CDI and in the percentage of cases due to ribotype 027 also coincided with the environmental cleaning initiative [7]. Mann-Kendall trend analysis demonstrated that the decreases in the CDI rate and in fluoroquinolone use were statistically significant in both the hospital and LTCF (P < 0.02). Hospital fluoroquinolone use was strongly correlated with the incidence of hospital-associated CDI (Pearson r = 0.79, 95% confidence interval 0.31-0.95; P < 0.01), but LTCF fluoroquinolone use was not correlated with LTCF-associated CDI (Pearson r = 0.29, 95% confidence interval -0.43-0.77; P = 0.44).
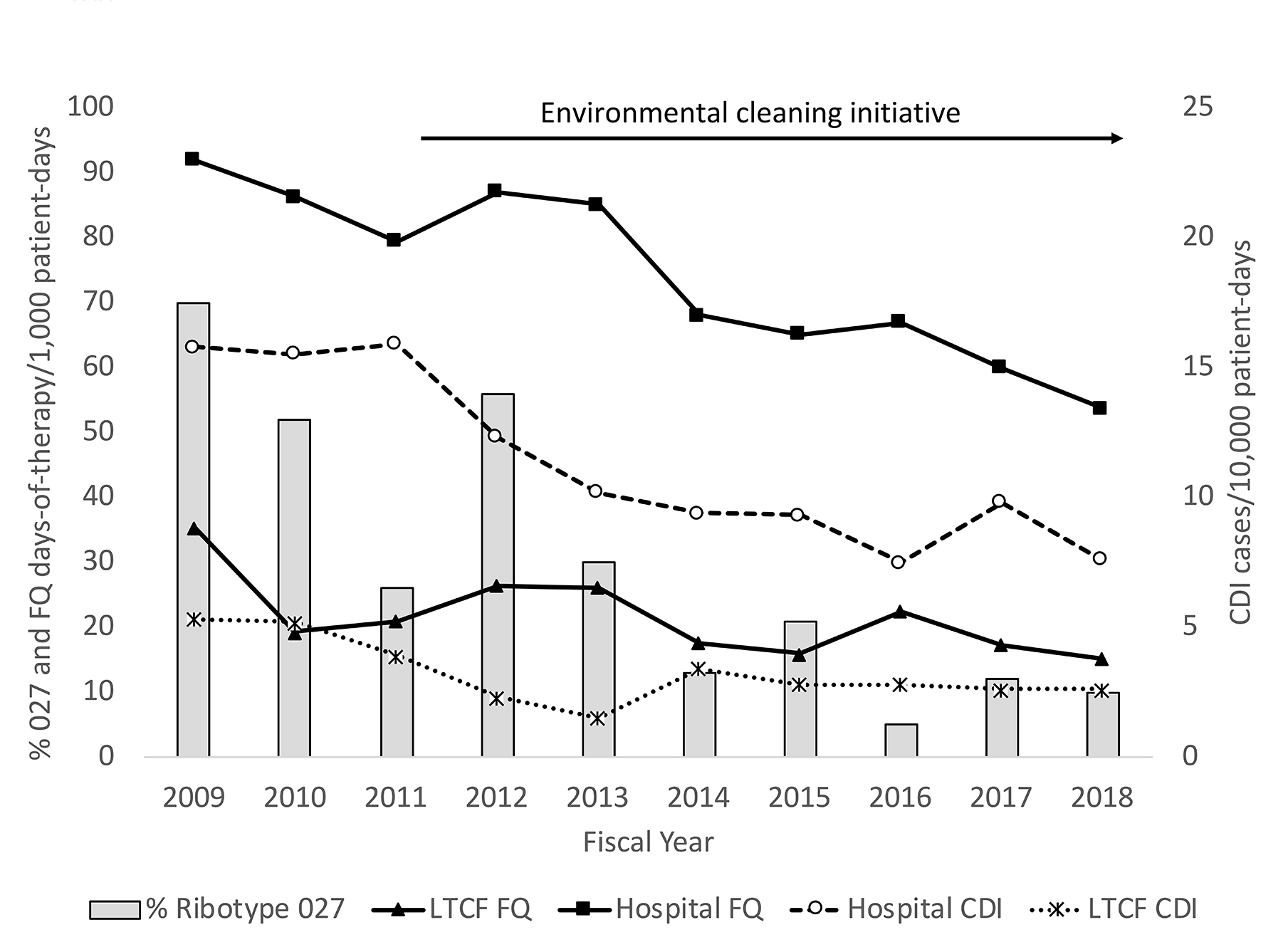
Figure 1. Changes in the incidence of hospital- and long-term care facility (LTCF)-associated Clostridioides difficile infection (CDI) and in the percentage of CDI infections due to ribotype 027 strains during a period of decreasing fluoroquinolone use. The environmental cleaning initiative resulted in reduced environmental contamination with C. difficile. Stewardship interventions also resulted in reductions in hospital use of penicillins, carbapenems, and intravenous vancomycin during the study period. Note. FQ, fluoroquinolone.
During the study period, hospital cephalosporin use increased by 45% (53 to 76 days-of-therapy per 1,000 patient-days), but the trend in use was not statistically significant (P = 0.86). There were statistically significant downward trends in the use of penicillins (17% decrease from 123 to 102 days-of-therapy per 1,000 patient-days, P < 0.01), intravenous vancomycin (36% decrease from 103 to 66 days-of-therapy per 1,000 patient-days, P < 0.01), carbapenems (44% decrease from 19 to 11 days-of-therapy per 1,000 patient-days; P < 0.01), and clindamycin (25% decrease from 4 to 3 days-of-therapy per 1,000 patient-days; P = 0.02). Macrolide use decreased by 18% from 22 to 18 days-of-therapy per 1,000 patient-days, but the trend in use was not statistically significant (P = 0.07).
Figure 2 shows the distribution of C. difficile ribotypes for 4 representative 1-year periods during the study. The decline in ribotype 027 was not associated with emergence of another predominant strain, rather a variety of strain types were detected. Strains that emerged included 014-020 and 078-126. Of 61 ribotype 027 isolates, 58 (95%) were moxifloxacin-resistant, including 29 (48%) that were highly resistant. Only 8 of 142 (6%) non-027 strains were fluoroquinolone resistant and none were highly resistant. The 8 fluoroquinolone-resistant non-027 isolates were from 6 different ribotypes including F053-163 (N = 2 isolates), F001 (N = 2 isolates), F017, F014-020, F002, and F198.
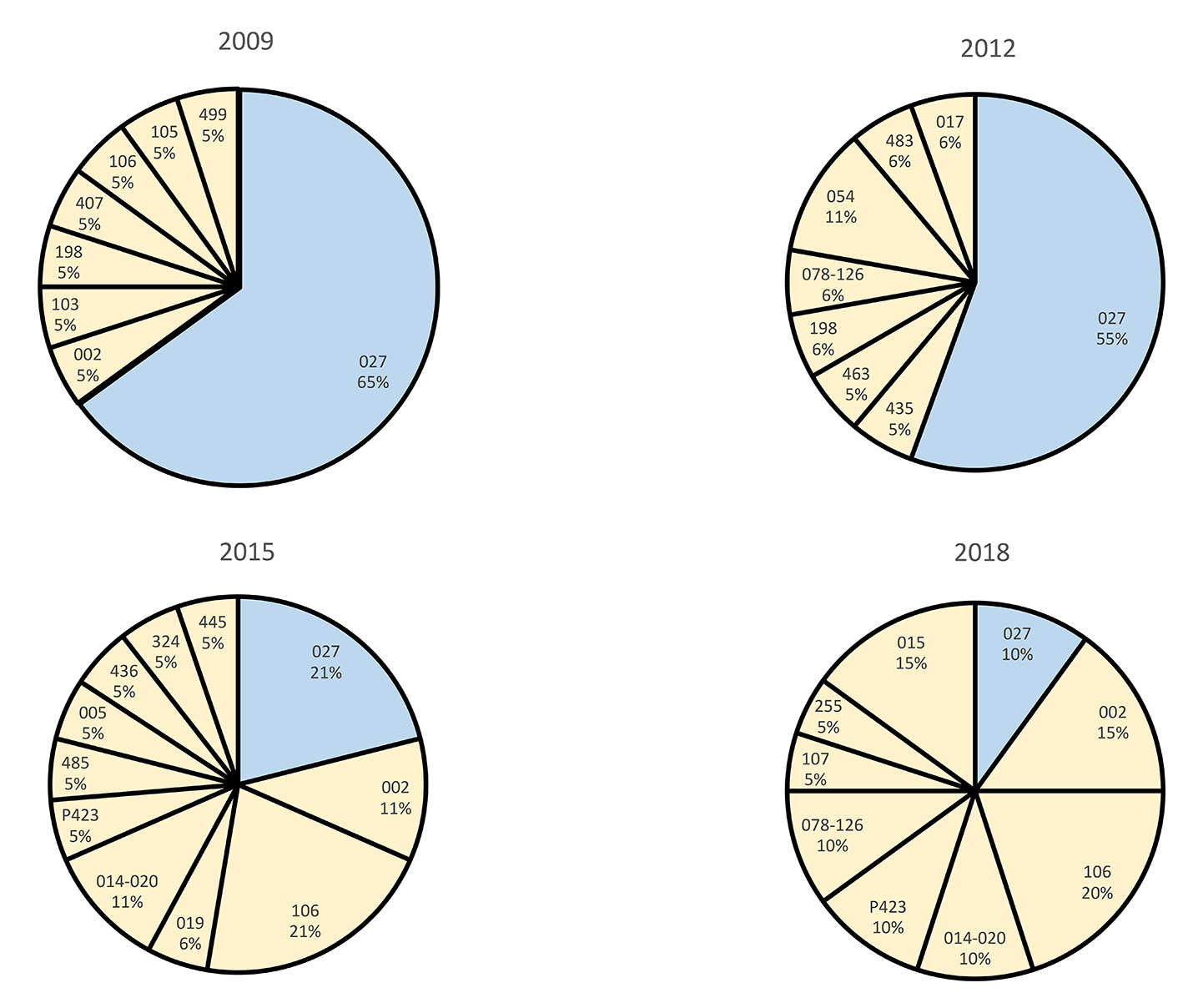
Figure 2. Distribution of polymerase chain reaction ribotypes of Clostridioides difficile isolates recovered from stool specimens testing positive for C. difficile during 4 representative years in a 10-year period. There were a total of 203 isolates (20 to 23 per year) subjected to ribotyping.
We found that antimicrobial stewardship interventions in our facility during the past decade have resulted in significant reductions in the use of fluoroquinolones, penicillins, carbapenems, and intravenous vancomycin, but not cephalosporins. An intervention to improve cleaning and disinfection was also effective in reducing environmental contamination with C. difficile [7]. We demonstrate that these interventions have been associated with reduced CDI incidence and a dramatic decrease in infections due to ribotype 027 strains. A majority of 027 strains tested were resistant to moxifloxacin, whereas only 6% of non-027 strains were moxifloxacin resistant.
Our findings provide support for fluoroquinolone restriction as a control measure for CDI, particularly in settings where epidemic 027 or other fluoroquinolone-resistant strains are common causes of infection. It is microbiologically plausible that the reduction in the 027 strain is attributable to reduced fluoroquinolone selective pressure. However, we cannot exclude the possibility that other factors may have contributed. If the 027 strain is more likely to spread or cause symptomatic disease, infection control interventions might have a disproportionate effect on these strains. In addition, epidemic C. difficile strains may decline in the absence of antibiotic restriction [3]. Recent data suggest that the prevalence of CDI due to the 027 strain may be decreasing throughout the VA healthcare system [8], and although fluoroquinolone use has decreased, this was not significant [9]. Previous quasi-experimental studies that have reported reductions in CDI and in the proportion of 027 strains in association with fluoroquinolone restriction have similar limitations as reductions in other antibiotic classes and improvements in cleaning occurred in conjunction with reductions in fluoroquinolones [3-4].
Although it is likely that antimicrobial stewardship interventions contributed substantially to the reduction in fluoroquinolone use in our facility, other factors could have played a role in reducing the use of these agents. Clinicians may have reduced prescription of fluoroquinolones in response to concerns about the risks associated with fluoroquinolones and awareness of increasing levels of resistance among Gram-negative pathogens in the facility. The US Food and Drug Administration (FDA) issued warnings regarding serious side effects associated with fluoroquinolones in 2008 and 2013 and enhanced warnings were published in 2016 [10]. The 2016 FDA communication recommended that fluoroquinolones should not be used for patients with acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, and uncomplicated urinary tract infections unless no alternative treatment options were available [10]. We have previously reported increasing rates of fluoroquinolone resistance among Escherichia coli urinary tract isolates from our facility [11-13]. Urologists and primary care providers were alerted to the problem of increasing fluoroquinolone resistance in 2010 due to an outbreak of infections with fluoroquinolone-resistant E. coli after transrectal ultrasound-guided prostate biopsy [11-12]. Others have reported reductions in the use of fluoroquinolones during the period of our study [9, 14-15].
In contrast to our findings, Hecker et al [5] reported that a similar reduction in fluoroquinolone prescribing in a tertiary care hospital was not associated with a reduction in the incidence of healthcare-associated CDI or in the proportion of cases due to 027 strains [5]. One potential explanation for the differing findings might be the difference in the setting of the studies or the patient populations. The study of Hecker et al [5] was conducted in a tertiary care level 1 trauma center receiving patients from many outside referral centers that might not have had similar reductions in fluoroquinolone use. The Cleveland VA Medical Center provides care for a more homogenous population and stewardship interventions and changes in practice patterns might be more likely to be implemented for the entire patient population. In addition, the baseline healthcare-associated CDI rate was substantially lower in the tertiary care hospital than in the Cleveland VA Medical Center [5]. It is plausible that reductions in antibiotic use might have a greater impact in settings with higher initial CDI rates.
Our study has some limitations. The study was conducted in a single healthcare facility with predominantly male and elderly patients. As noted previously, multiple potential confounding factors could have impacted CDI rates and the prevalence of 027 strains. We did not examine the appropriateness of fluoroquinolone therapy. However, substantial reductions in fluoroquinolone use may be feasible because these agents are often prescribed unnecessarily [5, 16].
We found that reductions in fluoroquinolone use were associated with reductions in the incidence of CDI and in infections due to ribotype 027 strains in a Veterans Affairs Medical Center. However, confounding factors such as reductions in other classes of antibiotics and improvements in environmental cleaning occurred during the study period. Thus, randomized trials are needed to clarify the effectiveness of fluoroquinolone restriction as a control measure for CDI.
We thank the Microbiology Laboratory and Pharmacy Service at the Cleveland VA Medical Center for assistance in obtaining the data and specimens used in the study.
This work was supported by a Merit Review grant from the Department of Veterans Affairs to C.J.D. (1-I01-CX-001848-01). The investigators were responsible for the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication. The funding agency was not involved in the study design, execution, analysis, interpretation, manuscript writing, or critique.
Dr. Donskey has received research funding from Clorox, Merck, GOJO, Pfizer, PDI, Avery Dennison, and Boehringer Laboratories. He is also an associate editor for Pathogens and Immunity.
1. McDonald LC, Killgore GE, Thompson A, Owens RC, Jr., Kazakova SV, Sambol SP, Johnson S, Gerding DN. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353(23):2433-41. PubMed PMID: 16322603. doi: 10.1056/NEJMoa05159
2. Wieczorkiewicz JT, Lopansri BK, Cheknis A, Osmolski JR, Hecht DW, Gerding DN, Johnson S. Fluoroquinolone and Macrolide Exposure Predict Clostridium difficile Infection with the Highly Fluoroquinolone- and Macrolide-Resistant Epidemic C. difficile Strain BI/NAP1/027. Antimicrob Agents Chemother. 2016;60(1):418-23. PubMed PMID: 26525793. Pubmed Central PMCID: 4704185. doi: 10.1128/AAC.01820-15
3. Donskey CJ. Fluoroquinolone restriction to control fluoroquinolone-resistant Clostridium difficile. Lancet Infect Dis. 2017;17(4):353-4. PubMed PMID: 28130062. doi: 10.1016/S1473-3099(17)30052-X
4. Dingle KE, Didelot X, Quan TP, Eyre DW, Stoesser N, Golubchik T, Harding RM, Wilson DJ, Griffiths D, Vaughan A, Finney JM, Wyllie DH, Oakley SJ, Fawley WN, Freeman J, Morris K, Martin J, Howard P, Gorbach S, Goldstein EJC, Citron DM, Hopkins S, Hope R, Johnson AP, Wilcox MH, Peto TEA, Walker AS, Crook DW, Modernising Medical Microbiology Informatics G. Effects of control interventions on Clostridium difficile infection in England: an observational study. Lancet Infect Dis. 2017;17(4):411-21. PubMed PMID: 28130063. Pubmed Central PMCID: 5368411. doi: 10.1016/S1473-3099(16)30514-X
5. Hecker MT, Son AH, Murphy NN, Sethi AK, Wilson BM, Watkins RR, Donskey CJ. Impact of syndrome-specific antimicrobial stewardship interventions on use of and resistance to fluoroquinolones: An interrupted time series analysis. Am J Infect Control. 2019;47(8):869-75. PubMed PMID: 30850252. doi: 10.1016/j.ajic.2019.01.026
6. Jump RL, Olds DM, Seifi N, Kypriotakis G, Jury LA, Peron EP, Hirsch AA, Drawz PE, Watts B, Bonomo RA, Donskey CJ. Effective antimicrobial stewardship in a long-term care facility through an infectious disease consultation service: keeping a LID on antibiotic use. Infect Control Hosp Epidemiol. 2012;33(12):1185-92. PubMed PMID: 23143354. Pubmed Central PMCID: 4370223. doi: 10.1086/668429
7. Sitzlar B, Deshpande A, Fertelli D, Kundrapu S, Sethi AK, Donskey CJ. An environmental disinfection odyssey: evaluation of sequential interventions to improve disinfection of Clostridium difficile isolation rooms. Infect Control Hosp Epidemiol. 2013;34(5):459-65. PubMed PMID: 23571361. doi: 10.1086/670217
8. Giancola SE, Williams RJ, 2nd, Gentry CA. Prevalence of the Clostridium difficile BI/NAP1/027 strain across the United States Veterans Health Administration. Clin Microbiol Infect. 2018;24(8):877-81. PubMed PMID: 29174729. doi: 10.1016/j.cmi.2017.11.011
9. Kelly AA, Jones MM, Echevarria KL, Kralovic SM, Samore MH, Goetz MB, Madaras-Kelly KJ, Simbartl LA, Morreale AP, Neuhauser MM, Roselle GA. A Report of the Efforts of the Veterans Health Administration National Antimicrobial Stewardship Initiative. Infect Control Hosp Epidemiol. 2017;38(5):513-20. PubMed PMID: 28118861. doi: 10.1017/ice.2016.328
10. FDA Drug Safety Communication: FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects. Food and Drug Administration website. https://www.fda.gov/downloads/Drugs/ DrugSafety/UCM513019.pdf. Published 2016. Accessed September 19, 2019.
11. Dumford D, 3rd, Suwantarat N, Bhasker V, Kundrapu S, Zabarsky TF, Drawz P, Zhu H, Donskey CJ. Outbreak of fluoroquinolone-resistant Escherichia coli infections after transrectal ultrasound-guided biopsy of the prostate. Infect Control Hosp Epidemiol. 2013;34(3):269-73. PubMed PMID: 23388361. doi: 10.1086/669512
12. Suwantarat N, Dumford DM, 3rd, Ponce-Terashima R, Kundrapu S, Zabarsky TF, Zhu H, Donskey CJ. Modification of antimicrobial prophylaxis based on rectal culture results to prevent fluoroquinolone-resistant Escherichia coli infections after prostate biopsy. Infect Control Hosp Epidemiol. 2013;34(9):973-6. PubMed PMID: 23917913. doi: 10.1086/671734
13. Suwantarat N, Rudin SD, Marshall SH, Hujer AM, Perez F, Hujer KM, Domitrovic TN, Dumford DM, 3rd, Donskey CJ, Bonomo RA. Infections caused by fluoroquinolone-resistant Escherichia coli following transrectal ultrasound-guided biopsy of the prostate. J Glob Antimicrob Resist. 2014;2(2):71-6. PubMed PMID: 25024933. Pubmed Central PMCID: 4093839. doi: 10.1016/j.jgar.2013.07.003
14. Yarrington ME, Anderson DJ, Dodds Ashley E, Jones T, Davis A, Johnson M, Lokhnygina Y, Sexton DJ, Moehring RW. Impact of FDA black box warning on fluoroquinolone and alternative antibiotic use in southeastern US hospitals. Infect Control Hosp Epidemiol. 2019:1-4. PubMed PMID: 31474240. doi: 10.1017/ice.2019.247
15. Almalki ZS, Yue X, Xia Y, Wigle PR, Guo JJ. Utilization, Spending, and Price Trends for Quinolones in the US Medicaid Programs: 25 Years' Experience 1991-2015. Pharmacoecon Open. 2017;1(2):123-31. PubMed PMID: 29442334. Pubmed Central PMCID: 5691846. doi: 10.1007/s41669-016-0007-y
16. Werner NL, Hecker MT, Sethi AK, Donskey CJ. Unnecessary use of fluoroquinolone antibiotics in hospitalized patients. BMC Infect Dis. 2011;11:187. PubMed PMID: 21729289. Pubmed Central PMCID: 3145580. doi: 10.1186/1471-2334-11-187